The CDC recently announced plans to reduce the recommended isolation period after testing positive for COVID from 5 days to just a single day, regardless of whether you continue to test positive. This decision isn’t grounded in a scientific finding, but rather in the perception that people are missing work or school because they are testing positive for COVID, and that COVID tests (but not COVID itself) are the problem. There seems to be a belief at the CDC that ignoring COVID test results will somehow lead to fewer sick days for students and workers. CDC representatives voiced concern that workers are missing out on pay when they test positive for COVID and stay home, and rather than advocating for paid sick leave, the CDC, alongside the public health agencies and governors of (Democratic) California and Oregon are issuing new guidelines to go to work, school, shopping, restaurants, etc., while knowingly contagious and testing positive for COVID. Masking recommendations remain unclear. So, people are going to find themselves in situations where they’re expected to be present despite being ill, potentially endangering others.
So, if future you gets sick with COVID and needs to take two weeks off because you sat next to a sniffling, sneezing, coughing colleague who tested positive for COVID the day prior, or if your asthmatic kid contracts COVID from a deskmate at school who was sent to class despite a positive COVID test– don’t be mad at them. They would be following the CDC’s new proposed recommendations to the letter, which are to come to work or school unless you have had a fever (defined by the CDC as a temperature of 100.5o F or higher) in the past 24 hours. CDC officials say that they want to bring their recommendations around COVID in line with existing recommendations about flu, and to treat COVID more like the flu and other respiratory illnesses.
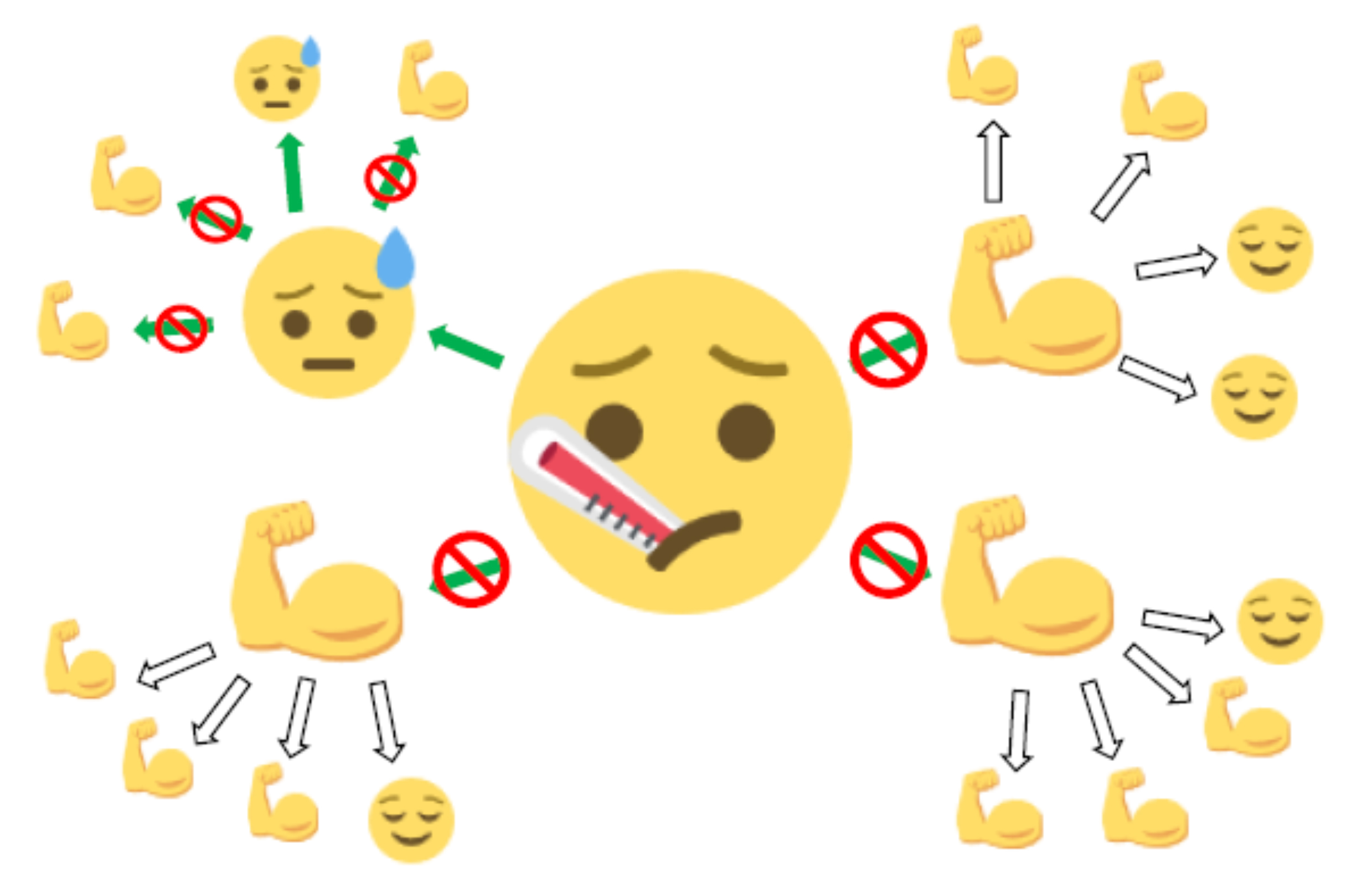
However, creating an equivalency between COVID and flu is misleading. Reasonable precautions against spreading the latter will not be effective for the former. Flu is characterized by rapid onset of a high fever, back and body aches, sore throat, cough, chills, and other symptoms. You can be contagious the day before symptoms start, and are most contagious the first 2-4 days you’re sick. Once your fever has been gone for 24 hours, there’s little chance of spreading the virus. COVID, on the other hand, presents with a wide spectrum of symptoms that only sometimes includes a clinical fever. Your first symptoms of a COVID infection can range from a runny nose to sore throat to vomiting or even neurological problems like dizziness and vertigo. You can be very contagious for 2-3 days before feeling sick, and it’s pretty common to remain contagious for 10 days, or even more, after symptom onset. Unlike the flu, where contagion risk diminishes once the fever subsides, COVID remains highly contagious even without fever. Thankfully, the development of affordable at-home COVID tests allow people to test to see if they have COVID when they’re feeling unwell, even if they don’t have a fever, and a positive test is a decent way to estimate if you’re contagious. Ignoring COVID test results and relying on fever as a determinant of contagion will almost certainly lead to increased spread of COVID.
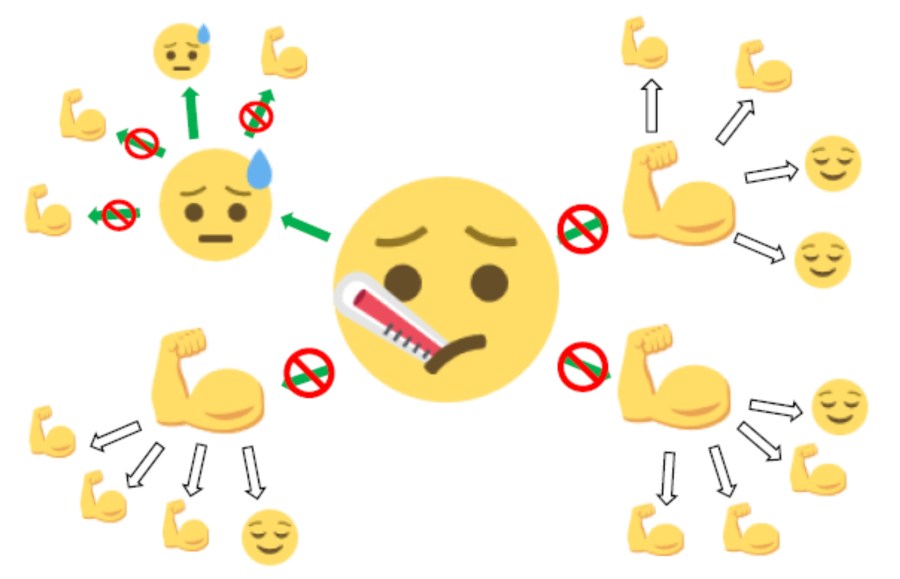
COVID and flu differ in a number of other important ways as well. COVID is 2-3 times more contagious than the flu. And about 4 times the number of people died with COVID vs flu in the 2022-2023 flu season. It seems like this will be the case for this year as well (recent weeks have seen about 500-700 deaths per week with flu, compared with about 2000-2300 with COVID).
Additionally, a frequent complication of COVID is Long COVID, a chronic condition that can be disabling, even for young and previously healthy people. Data indicates that 7% of Americans have experienced Long COVID– that’s over 20 million people.
I’m one of them. Long COVID derailed my life after I contracted COVID in March of 2020. I work today with other people who have Long COVID, and I wish I could say that vaccination eliminates the risk of Long COVID, or that no one gets Long COVID from Omicron strains of the virus– but this just is not true. There are new people developing Long COVID and reaching out for help every day, even now, even people who have been vaccinated or who have fully recovered from previous COVID infections. The CDC knows this.
COVID isn’t the first or only infectious disease that causes long-lasting illness or disability. I grew up around older family members who spoke about diseases like polio, whooping cough, typhoid, lockjaw, scarlet fever, mumps, and measles. They spoke of victims and survivors of these in the same tones as they spoke of the world wars. The loss and devastation that followed these infections was measured not only in deaths, but in lives characterized by the abrupt onset of chronic illness and disability following infection. They wondered sometimes why they had been spared when their loved ones had not.

who was born in 1899.
The development of the vaccinations and treatments that have largely eradicated these plagues from America seems now to have had the unfortunate side effect of having also eradicated lived knowledge of the prevalence of serious post-infectious conditions. For many Americans the flu is the only infection they have lived experience of prior to COVID, and so it’s the only COVID comparison they reach for, as inaccurate as it is. Public health agencies, however, should know not to do so.
The CDC has not yet officially released these guidelines; I still hope that more rational thinking and evidence-based policies will prevail. Throughout the history of public health, successful control of pathogens has relied the use of all the tools provided by science, and gaining public trust through steadfast communication of accurate scientific guidance. It’s important to continue to do so now.